Irregular Periods: When to Worry & When It’s Normal
Clinically reviewed by: Dr. Nitasha Gupta – Consultant Gynecologist, IVF & Women’s Health Specialist
Menstrual cycles are a vital sign of a woman’s hormonal and reproductive health. While most women expect periods every 28 days, the truth is that normal menstrual cycles can range from 21 to 35 days. Occasional changes may be harmless — but persistent irregular periods can signal underlying medical conditions that need attention.
This comprehensive guide explains what irregular periods are, why they happen, when to worry, and when to consult a gynecologist, based on clinical experience and evidence-based medicine.
Contents
- Overview
- Symptoms & Causes
- Diagnosis & Tests
- Management & Treatment
- Prevention
- Living With Irregular Periods
- Frequently Asked Questions
What Are Irregular Periods?
Irregular periods refer to menstrual cycles that vary significantly in timing, duration, or flow. While minor cycle variation is normal, persistent irregular menstruation may indicate hormonal imbalance, gynecological disorders, or metabolic issues.
Examples of Irregular Periods
- Periods occurring less than 21 days or more than 35 days apart
- Missing three or more periods in a row
- Extremely heavy or very light menstrual bleeding
- Periods lasting longer than seven days
- Bleeding or spotting between periods or after intercourse
- Severe pain, nausea, or vomiting during periods
Medical Conditions Associated With Irregular Periods
- Amenorrhea: Absence of periods for 90 days or more
- Oligomenorrhea: Infrequent menstrual cycles
- Dysmenorrhea: Painful periods with severe cramps
- Abnormal Uterine Bleeding
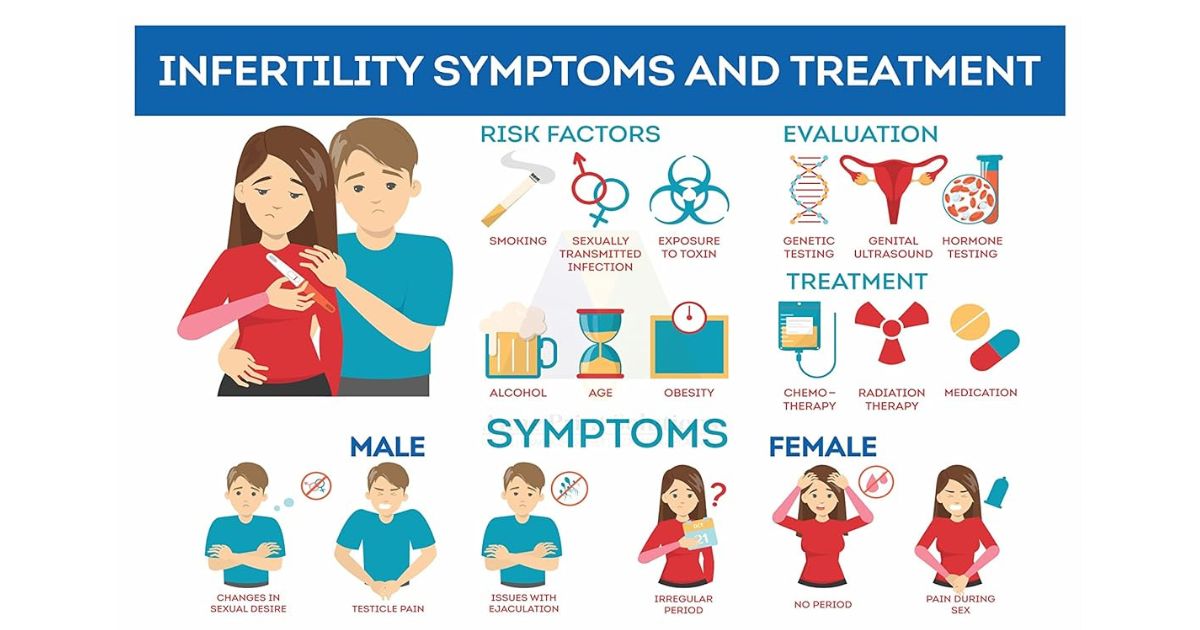
Conditions such as PCOS, endometriosis, thyroid disorders, and premature ovarian insufficiency are common causes of irregular periods.
Symptoms & Causes of Irregular Periods
Medical Causes
- Polycystic Ovary Syndrome (PCOS)
- Endometriosis
- Pelvic Inflammatory Disease (PID)
- Thyroid or pituitary gland disorders
- Bleeding or clotting disorders
- Uterine fibroids or ovarian cysts
Lifestyle & Hormonal Causes
- Chronic stress
- Rapid weight gain or weight loss
- Excessive exercise or low body fat
- Hormonal contraceptive use
- Post-pregnancy or breastfeeding changes
Diagnosis and Tests
Diagnosing irregular periods requires a detailed menstrual history, physical examination, and targeted investigations.
- Pelvic ultrasound
- Hormonal blood tests
- Endometrial biopsy
- Hysteroscopy
Diagnosis and Tests
Diagnosing irregular periods requires a detailed menstrual history, physical examination, and targeted investigations.
- Pelvic ultrasound
- Hormonal blood tests
- Endometrial biopsy
- Hysteroscopy
Management and Treatment Options
Medical Treatment
- Hormonal therapy or birth control pills
- Tranexamic acid for heavy bleeding
- Pain relievers (NSAIDs)
- Antibiotics for infections
Surgical Options (If Required)
- Endometrial ablation
- Myomectomy
- Uterine artery embolization
- Hysterectomy (rare cases)
How to Reduce the Risk of Irregular Periods
- Maintain a healthy weight
- Manage stress effectively
- Avoid extreme dieting or over-exercising
- Follow contraceptive instructions carefully
- Schedule regular gynecological check-ups
When Should You See a Gynecologist?
Consult a gynecologist immediately if you experience:
- Severe pelvic pain
- Heavy bleeding soaking pads every hour
- Periods lasting longer than seven days
- Bleeding after menopause
- Missed periods for more than three months
Frequently Asked Questions
Is it normal to miss a period for two months?
Occasional missed periods may be due to stress or lifestyle changes, but missing three or more periods requires medical evaluation.
How much delay in periods is normal?
A variation of a few days is normal. Sudden or persistent changes should be checked by a gynecologist.
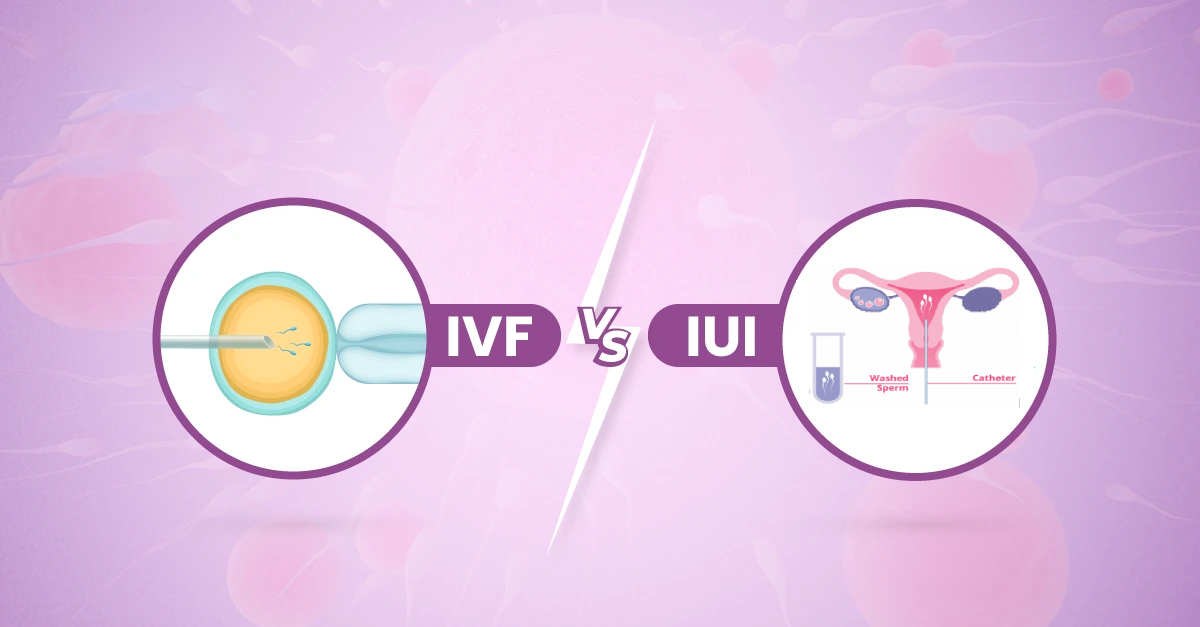
Can irregular periods affect fertility?
Yes. Irregular ovulation can make conception difficult. Early treatment improves fertility outcomes.
When are irregular periods most common?
They are common during adolescence and perimenopause.
Medical references:
Cleveland Clinic |
ACOG
If you’re experiencing irregular periods and want expert evaluation, book a consultation with
Dr. Nitasha Gupta, trusted gynecologist and fertility specialist.